Can You Have a Sinus Infection Without Mucus
| Sinusitis | |
|---|---|
| Other names | Sinus infection, rhinosinusitis |
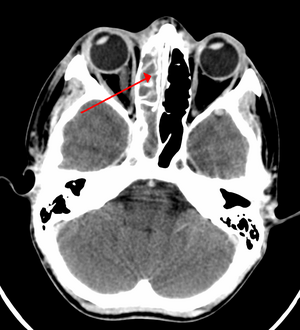 | |
| A CT scan showing sinusitis of the ethmoid sinus | |
| Specialty | Otorhinolaryngology |
| Symptoms | Thick nasal mucus, plugged nose, pain in the face, fever[ane] [2] |
| Causes | Infection (bacterial, fungal, viral), allergies, air pollution, structural bug in the nose[two] |
| Risk factors | Asthma, cystic fibrosis, poor immune function[1] |
| Diagnostic method | Usually based on symptoms[1] |
| Differential diagnosis | Migraine[3] |
| Prevention | Handwashing, avoiding smoking |
| Treatment | Pain medications, nasal steroids, nasal irrigation, antibody[1] [four] |
| Frequency | 10–30% each twelvemonth (developed globe)[1] [5] |
Sinusitis, also known every bit rhinosinusitis, is inflammation of the mucous membranes that line the sinuses resulting in symptoms that may include thick nasal mucus, a plugged nose, and facial hurting.[1] [half dozen] Other signs and symptoms may include fever, headaches, a poor sense of olfactory property, sore pharynx, and a coughing.[2] Information technology is defined as acute sinusitis if information technology lasts less than four weeks, and as chronic sinusitis if information technology lasts for more than 12 weeks.[ane]
Sinusitis can be caused by infection, allergies, air pollution, or structural bug in the nose.[2] Almost cases are caused by a viral infection.[ii] Recurrent episodes are more likely in persons with asthma, cystic fibrosis, and poor allowed function.[1] X-rays are not usually needed unless complications are suspected.[1] In chronic cases, confirmatory testing is recommended past either directly visualization or computed tomography.[1]
Some cases may be prevented past hand washing, avoiding smoking, and immunization.[ii] Pain killers such equally naproxen, nasal steroids, and nasal irrigation may be used to help with symptoms.[1] [iv] Recommended initial treatment for acute sinusitis is watchful waiting.[i] If symptoms exercise non improve in vii–ten days or get worse, and then an antibiotic may be used or inverse.[1] In those in whom antibiotics are used, either amoxicillin or amoxicillin/clavulanate is recommended beginning line.[1] Surgery may occasionally be used in people with chronic disease.[vii]
Sinusitis is a common condition.[1] It affects between almost 10 and thirty percent of people each year in the U.s.a. and Europe.[1] [5] Chronic sinusitis affects about 12.5% of people.[8] Treatment of sinusitis in the United states results in more than US$11 billion in costs.[1] The unnecessary and ineffective treatment of viral sinusitis with antibiotics is common.[1]
Signs and symptoms [edit]
Headache, facial pain, or pressure of a wearisome, constant, or aching sort over the affected sinuses is mutual with both acute and chronic stages of sinusitis. This pain is usually localized to the involved sinus and may worsen when the afflicted person bends over or lies down. Pain often starts on i side of the head and progresses to both sides.[9] Acute sinusitis may exist accompanied by a thick nasal discharge that is usually greenish in color, and may contain pus or blood.[10] Often, a localized headache or toothache is present, and these symptoms distinguish a sinus-related headache from other types of headaches, such as tension and migraine headaches. Some other way to distinguish between toothache and sinusitis is that the pain in sinusitis is usually worsened by tilting the head frontwards and with the Valsalva maneuver.[xi]
Other symptoms associated with acute rhinosinusitis include cough, fatigue, hyposmia, anosmia and ear fullness or pressure.[12]
Sinus infections can also cause middle-ear bug due to the congestion of the nasal passages. This can be demonstrated past dizziness, "a pressurized or heavy head", or vibrating sensations in the head. Postnasal baste is also a symptom of chronic rhinosinusitis.
Halitosis (bad jiff) is often stated to be a symptom of chronic rhinosinusitis; all the same, gold-standard jiff assay techniques[ clarification needed ] have not been applied. Theoretically, several possible mechanisms of both objective and subjective halitosis may be involved.[11]
A 2005 review suggested that most "sinus headaches" are migraines.[thirteen] The defoliation occurs in part considering migraine involves activation of the trigeminal nerves, which innervate both the sinus region and the meninges surrounding the brain. As a effect, accurately determining the site from which the pain originates is difficult. People with migraines do not typically accept the thick nasal belch that is a common symptom of a sinus infection.[14]
Symptoms of chronic sinusitis may include nasal congestion, facial pain, headache, night-time coughing, an increase in previously minor or controlled asthma symptoms, general malaise, thick green or yellow discharge, feeling of facial fullness or tightness that may worsen when bending over, dizziness, aching teeth, and bad breath.[15] Oft, chronic sinusitis can lead to anosmia, the loss of the sense of smell.[fifteen]
By location [edit]
The four paired paranasal sinuses are the frontal, ethmoidal, maxillary, and sphenoidal sinuses. The ethmoidal sinuses are further subdivided into anterior and posterior ethmoid sinuses, the division of which is defined as the basal lamella of the heart nasal concha. In improver to the severity of affliction, discussed below, sinusitis can be classified by the sinus cavity it affects:
- Maxillary – tin can cause hurting or force per unit area in the maxillary (cheek) area (e.grand., toothache,[11] or headache) (J01.0/J32.0)
- Frontal – can cause hurting or pressure in the frontal sinus crenel (located above the eyes), headache, specially in the forehead (J01.1/J32.1)
- Ethmoidal – can cause pain or pressure pain betwixt/behind the eyes, the sides of the upper role of the nose (the medial canthi), and headaches (J01.2/J32.2)[16]
- Sphenoidal – can cause pain or pressure level backside the optics, but is often felt in the elevation of the caput, over the mastoid processes, or the back of the head.[16]
Complications [edit]
| Stage | Clarification |
|---|---|
| I | Preseptal cellulitis |
| II | Orbital cellulitis |
| III | Subperiosteal abscess |
| IV | Orbital abscess |
| 5 | Cavernous sinus septic thrombosis |
Complications are thought to be rare (1 case per 10,000).[17]
The proximity of the encephalon to the sinuses makes the most unsafe complication of sinusitis, particularly involving the frontal and sphenoid sinuses, infection of the brain past the invasion of anaerobic bacteria through the basic or blood vessels. Abscesses, meningitis, and other life-threatening weather condition may result. In extreme cases, the patient may experience balmy personality changes, headache, altered consciousness, visual issues, seizures, coma, and possibly death.[9]
Sinus infection can spread through anastomosing veins or by direct extension to shut structures. Orbital complications were categorized by Chandler et al. into five stages according to their severity (see table).[18] Face-to-face spread to the orbit may issue in periorbital cellulitis, subperiosteal abscess, orbital cellulitis, and abscess. Orbital cellulitis can complicate astute ethmoiditis if anterior and posterior ethmoidal veins thrombophlebitis enables the spread of the infection to the lateral or orbital side of the ethmoid labyrinth. Sinusitis may extend to the central nervous system, where it may cause clangorous sinus thrombosis, retrograde meningitis, and epidural, subdural, and brain abscesses.[nineteen] Orbital symptoms frequently precede intracranial spread of the infection . Other complications include sinobronchitis, maxillary osteomyelitis, and frontal bone osteomyelitis.[20] [21] [22] [23] Osteomyelitis of the frontal os often originates from a spreading thrombophlebitis. A periostitis of the frontal sinus causes an osteitis and a periostitis of the outer membrane, which produces a tender, puffy swelling of the forehead.[ commendation needed ]
The diagnosis of these complications can be assisted by noting local tenderness and dull hurting, and can exist confirmed by CT and nuclear isotope scanning. The well-nigh common microbial causes are anaerobic bacteria and S. aureus. Treatment includes performing surgical drainage and assistants of antimicrobial therapy. Surgical debridement is rarely required afterward an extended course of parenteral antimicrobial therapy.[24] Chronic sinus infections may pb to rima oris breathing, which can result in oral fissure dryness and an increased hazard of gingivitis. Decongestants may too cause oral fissure dryness.[25]
If an odontogenic infection involves the maxillary sinus, odontogenic sinusitis (ODS) may ensue.[26] Odontogenic sinusitis tin can often spread to other sinuses such equally the ethmoid, frontal and (less ofttimes) sphenoid sinus, and even to the contralateral nasal cavity.[27] In rare instances, these infections may involve the orbit, causing orbital cellulitis, which may in plow result in blindness, or make up one's mind central nervous system complications such equally meningitis, subdural empyema, encephalon abscess and life-threatening cavernous sinus thrombosis.[28] [29]
Infection of the eye socket is a rare complication of ethmoid sinusitis, which may result in the loss of sight and is accompanied by fever and astringent illness. Another possible complexity is the infection of the bones (osteomyelitis) of the forehead and other facial bones – Pott's puffy tumor.[9]
Causes [edit]
Maxillary sinusitis may besides develop from issues with the teeth, and these cases were calculated to exist about 40% in i report and fifty% in some other.[29] The cause of this situation is unremarkably a periapical or periodontal infection of a maxillary posterior molar, where the inflammatory exudate has eroded through the bone superiorly to bleed into the maxillary sinus.[29]
An estimated 0.v to 2.0% of viral rhinosinusitis (VRS) will develop into bacterial infections in adults and 5 to 10% in children.[12]
Acute [edit]
Acute sinusitis is usually precipitated by an earlier upper respiratory tract infection, generally of viral origin, by and large caused by rhinoviruses (with RVA and RVC giving more severe infection than RVB), coronaviruses, and influenza viruses, others caused past adenoviruses, human parainfluenza viruses, man respiratory syncytial virus, enteroviruses other than rhinoviruses, and metapneumovirus. If the infection is of bacterial origin, the most common three causative agents are Streptococcus pneumoniae (38%), Haemophilus influenzae (36%), and Moraxella catarrhalis (16%).[12] [thirty] Until recently, H. influenzae was the most common bacterial agent to cause sinus infections. However, introduction of the H. influenzae type B (Hib) vaccine has dramatically decreased these infections and now non-typable H. influenzae (NTHI) is predominantly seen in clinics. Other sinusitis-causing bacterial pathogens include S. aureus and other streptococci species, anaerobic leaner and, less ordinarily, Gram-negative bacteria. Viral sinusitis typically lasts for 7 to ten days.[17]
Acute episodes of sinusitis tin also result from fungal invasion. These infections are typically seen in people with diabetes or other immune deficiencies (such equally AIDS or transplant on immunosuppressive antirejection medications) and can be life-threatening. In blazon I diabetics, ketoacidosis can be associated with sinusitis due to mucormycosis.[31]
Chronic [edit]
By definition, chronic sinusitis lasts longer than 12 weeks and tin be caused past many dissimilar diseases that share chronic inflammation of the sinuses as a common symptom. It is subdivided into cases with and without polyps. When polyps are present, the condition is chosen chronic hyperplastic sinusitis; however, the causes are poorly understood.[17] It may develop with anatomic derangements, including deviation of the nasal septum and the presence of concha bullosa (pneumatization of the center concha) that inhibit the outflow of mucus, or with allergic rhinitis, asthma, cystic fibrosis, and dental infections.[32]
Chronic rhinosinusitis represents a multifactorial inflammatory disorder, rather than merely a persistent bacterial infection.[17] The medical management of chronic rhinosinusitis is at present focused upon controlling the inflammation that predisposes people to obstruction, reducing the incidence of infections.[33] Surgery may be needed if medications are not working.[33]
Attempts take been fabricated to provide a more consequent nomenclature for subtypes of chronic sinusitis. The presence of eosinophils in the mucous lining of the olfactory organ and paranasal sinuses has been demonstrated for many people, and this has been termed eosinophilic mucin rhinosinusitis (EMRS). Cases of EMRS may be related to an allergic response, but allergy is non oft documented, resulting in further subcategorization into allergic and nonallergic EMRS.[34]
A more recent, and notwithstanding debated, evolution in chronic sinusitis is the part that fungi play in this illness.[35] Whether fungi are a definite factor in the evolution of chronic sinusitis remains unclear, and if they are, what is the difference betwixt those who develop the illness and those who remain free of symptoms. Trials of antifungal treatments have had mixed results.[36]
Recent theories of sinusitis indicate that information technology often occurs as part of a spectrum of diseases that bear on the respiratory tract (i.e., the "one airway" theory) and is frequently linked to asthma.[37] [38]
Both smoking and secondhand fume are associated with chronic rhinosinusitis.[8]
Other diseases such as cystic fibrosis and granulomatosis with polyangiitis tin can likewise cause chronic sinusitis.[39]
Pathophysiology [edit]
Biofilm bacterial infections may business relationship for many cases of antibiotic-refractory chronic sinusitis.[40] [41] [42] Biofilms are complex aggregates of extracellular matrix and interdependent microorganisms from multiple species, many of which may be difficult or incommunicable to isolate using standard clinical laboratory techniques.[43] Bacteria found in biofilms have their antibiotic resistance increased up to 1000 times when compared to gratis-living bacteria of the same species. A recent study establish that biofilms were present on the mucosa of 75% of people undergoing surgery for chronic sinusitis.[44]
Diagnosis [edit]
Classification [edit]

Analogy depicting sinusitis
Sinusitis (or rhinosinusitis) is divers as an inflammation of the mucous membrane that lines the paranasal sinuses and is classified chronologically into several categories:[15]
- Acute sinusitis – A new infection that may terminal up to four weeks and can exist subdivided symptomatically into severe and nonsevere. Some use definitions up to 12 weeks.[one]
- Recurrent acute sinusitis – Four or more total episodes of acute sinusitis that occur within i twelvemonth
- Subacute sinusitis – An infection that lasts between four and 12 weeks, and represents a transition between astute and chronic infection
- Chronic sinusitis – When the signs and symptoms last for more than than 12 weeks.[1]
- Astute exacerbation of chronic sinusitis – When the signs and symptoms of chronic sinusitis exacerbate, but return to baseline after handling
Roughly 90% of adults have had sinusitis at some betoken in their lives.[45]
Astute [edit]
Health care providers distinguish bacterial and viral sinusitis past watchful waiting.[one] If a person has had sinusitis for fewer than 10 days without the symptoms condign worse, and so the infection is presumed to be viral.[i] When symptoms last more than 10 days or get worse in that time, so the infection is considered bacterial sinusitis.[46] Pain in the teeth and bad breath are also more than indicative of bacterial disease.[47]
Imaging past either Ten-ray, CT or MRI is generally not recommended unless complications develop.[46] Hurting acquired past sinusitis is sometimes confused for pain caused by pulpitis (toothache) of the maxillary teeth, and vice versa. Classically, the increased pain when tilting the head forwards separates sinusitis from pulpitis.[ commendation needed ]
For cases of maxillary sinusitis, limited field CBCT imaging, equally compared to periapical radiographs, improves the power to detect the teeth as the sources for sinusitis. A coronal CT picture may likewise be useful.[29]
Chronic [edit]
For sinusitis lasting more than than 12 weeks, a CT scan is recommended.[46] On a CT scan, acute sinus secretions have a radiodensity of ten to 25 Hounsfield units (HU), but in a more chronic state they become more viscous, with a radiodensity of 30 to 60 HU.[48]
Nasal endoscopy and clinical symptoms are also used to make a positive diagnosis.[17] A tissue sample for histology and cultures can besides exist collected and tested.[49] Nasal endoscopy involves inserting a flexible fiber-optic tube with a calorie-free and camera at its tip into the nose to examine the nasal passages and sinuses.
Sinus infections, if they upshot in tooth pain, unremarkably present with pain involving more i of the upper teeth, whereas a toothache normally involves a single molar. Dental examination and appropriate radiography help in ruling out pain arises from a tooth.[25]
-

CT of chronic sinusitis
-

CT scan of chronic sinusitis, showing a filled right maxillary sinus with sclerotic thickened bone.
-

MRI image showing sinusitis. Edema and mucosal thickening appears in both maxillary sinuses.
-

Frontal sinusitis
-

X-ray of left-sided maxillary sinusitis marked by an pointer. There is lack of the air transparency indicating fluid in dissimilarity to the other side.
Treatment [edit]
| Treatments[50] [51] | ||
|---|---|---|
| Handling | Indication | Rationale |
| Time | Viral and some bacterial sinusitis | Sinusitis is usually caused by a virus which is not affected past antibiotics.[50] |
| Antibiotics | Bacterial sinusitis | Cases accompanied by extreme pain, skin infection, or which last a long time may be caused by bacteria.[50] |
| Nasal irrigation | Nasal congestion | Can provide relief by helping decongest.[50] |
| Drink liquids | Thick phlegm | Remaining hydrated loosens mucus.[l] |
| Antihistamines | Concern with allergies | Antihistamines do not relieve typical sinusitis or cold symptoms much; this treatment is not needed in most cases.[l] |
| Nasal spray | Desire for temporary relief | Tentative evidence that it helps symptoms.[four] Does not treat cause. Non recommended for more than than three days' utilise.[50] |
Recommended treatments for most cases of sinusitis include rest and drinking plenty water to sparse the mucus.[52] Antibiotics are not recommended for most cases.[52] [53]
Breathing low-temperature steam such as from a hot shower or gargling can salvage symptoms.[52] [54] There is tentative show for nasal irrigation in acute sinusitis, for instance during upper respiratory infections.[4] Decongestant nasal sprays containing oxymetazoline may provide relief, but these medications should not exist used for more than the recommended period. Longer use may cause rebound sinusitis.[55] Information technology is unclear if nasal irrigation, antihistamines, or decongestants work in children with astute sinusitis.[56] There is no clear show that plant extracts such as Cyclamen europaeum are effective as an intranasal launder to treat acute sinusitis.[57] Evidence is inconclusive on whether anti-fungal treatments improve symptoms or quality of life.[58]
Antibiotics [edit]
Near sinusitis cases are caused by viruses and resolve without antibiotics.[17] Yet, if symptoms exercise not resolve within 10 days, amoxicillin/clavulanate is a reasonable antibiotic association for first handling.[17] A 2022 Cochrane review, however, plant no evidence that people with symptoms lasting seven days or more before consulting their physician are more probable to accept bacterial sinusitis as 1 study constitute that about 80% of patients accept symptoms lasting more than vii days and another about 70%.[59] Antibiotics are specifically not recommended in those with mild / moderate illness during the first week of infection due to risk of adverse effects, antibody resistance, and cost.[60]
Fluoroquinolones, and a newer macrolide antibiotic such as clarithromycin or a tetracycline similar doxycycline, are used in those who have severe allergies to penicillins.[61] Because of increasing resistance to amoxicillin the 2012 guideline of the Infectious Diseases Lodge of America recommends amoxicillin-clavulanate as the initial treatment of choice for bacterial sinusitis.[62] The guidelines also recommend against other commonly used antibiotics, including azithromycin, clarithromycin, and trimethoprim/sulfamethoxazole, considering of growing antibiotic resistance. The FDA recommends against the use of fluoroquinolones when other options are available due to college risks of serious side effects.[63]
A curt-course (3–7 days) of antibiotics seems to exist simply as effective as the typical longer-class (x–14 days) of antibiotics for those with clinically diagnosed acute bacterial sinusitis without any other astringent disease or complicating factors.[64] The IDSA guideline propose v to seven days of antibiotics is long enough to treat a bacterial infection without encouraging resistance. The guidelines still recommend children receive antibody handling for ten days to two weeks.[62]
Corticosteroids [edit]
For unconfirmed acute sinusitis, nasal sprays using corticosteroids have non been constitute to be better than a placebo either lonely or in combination with antibiotics.[65] For cases confirmed by radiology or nasal endoscopy, treatment with intranasal corticosteroids alone or in combination with antibiotics is supported.[66] The benefit, all the same, is minor.[67]
For confirmed chronic rhinosinusitis, there is express evidence that intranasal steroids improve symptoms and insufficient show that one type of steroid is more effective.[68] [69]
There is only limited show to support short treatment with corticosteroids by oral fissure for chronic rhinosinusitis with nasal polyps.[70] [71] [72] In that location is limited evidence to back up corticosteroids by mouth in combination with antibiotics for acute sinusitis; it has merely brusque-term consequence improving the symptoms.[73] [74]
Surgery [edit]
For sinusitis of dental origin, treatment focuses on removing the infection and preventing reinfection, by removal of the microorganisms, their byproducts, and pulpal debris from the infected root canal.[29] Systemic antibiotics are ineffective as a definitive solution, but may afford temporary relief of symptoms by improving sinus clearing, and may be appropriate for rapidly spreading infections, merely debridement and disinfection of the root culvert organisation at the same time is necessary. Treatment options include non-surgical root canal treatment, periradicular surgery, tooth replantation, or extraction of the infected tooth.[29]
For chronic or recurring sinusitis, referral to an otolaryngologist may be indicated, and treatment options may include nasal surgery. Surgery should just be considered for those people who do not do good with medication.[71] [75] It is unclear how benefits of surgery compare to medical treatments in those with nasal polyps equally this has been poorly studied.[76] [77]
A number of surgical approaches can be used to access the sinuses and these accept generally shifted from external/extranasal approaches to intranasal endoscopic ones. The benefit of functional endoscopic sinus surgery (FESS) is its ability to let for a more than targeted arroyo to the affected sinuses, reducing tissue disruption, and minimizing post-operative complications.[78] The utilize of drug eluting stents such equally propel mometasone furoate implant may help in recovery later surgery.[79]
Some other recently adult handling is balloon sinuplasty. This method, similar to balloon angioplasty used to "unclog" arteries of the middle, utilizes balloons in an attempt to expand the openings of the sinuses in a less invasive manner.[33] The effectiveness of the functional endoscopic balloon dilation arroyo compared to conventional FESS is not known.[33]
Treatments directed to rhinovirus infection [edit]
A study has shown that patients given spray formulation of 0.73 mg of Tremacamra (a soluble intercellular adhesion molecule 1 [ICAM-1] receptor) reduced the severity of disease.[30]
Prognosis [edit]
A 2022 review has found that without the utilize of antibiotics, about 46% were cured after i week and 64% after ii weeks.[59]
Epidemiology [edit]
Sinusitis is a common condition, with betwixt 24 and 31 million cases occurring in the United States annually.[80] [81] Chronic sinusitis affects approximately 12.5% of people.[8]
Research [edit]
Based on recent theories on the part that fungi may play in the development of chronic sinusitis, antifungal treatments accept been used, on a trial basis. These trials have had mixed results.[17]
Come across also [edit]
- Fungal sinusitis
References [edit]
- ^ a b c d e f 1000 h i j one thousand l m due north o p q r south t u five Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Beck I, Kumar KA, Kramper M, Orlandi RR, Palmer JN, Patel ZM, Peters A, Walsh SA, Corrigan MD (April 2015). "Clinical do guideline (update): Adult Sinusitis Executive Summary". Otolaryngology–Head and Neck Surgery. 152 (4): 598–609. doi:10.1177/0194599815574247. PMID 25833927. S2CID 206469424.
- ^ a b c d east f "Sinus Infection (Sinusitis)". cdc.gov. September xxx, 2013. Archived from the original on 7 April 2015. Retrieved vi April 2015.
- ^ "Migraines vs. Sinus Headaches". American Migraine Foundation . Retrieved 2017-ten-23 .
- ^ a b c d King D, Mitchell B, Williams CP, Spurling GK (Apr 2015). "Saline nasal irrigation for acute upper respiratory tract infections" (PDF). The Cochrane Database of Systematic Reviews. 4 (4): CD006821. doi:10.1002/14651858.CD006821.pub3. PMID 25892369.
- ^ a b Adkinson NF (2014). Middleton'southward allergy: principles and exercise (Eight ed.). Philadelphia: Elsevier Saunders. p. 687. ISBN9780323085939. Archived from the original on 2016-06-03.
- ^ Head K, Chong LY, Piromchai P, Hopkins C, Philpott C, Schilder AG, Burton MJ (April 2016). "Systemic and topical antibiotics for chronic rhinosinusitis" (PDF). The Cochrane Database of Systematic Reviews. 4: CD011994. doi:10.1002/14651858.CD011994.pub2. PMID 27113482.
- ^ "How Is Sinusitis Treated?". April three, 2012. Archived from the original on 5 April 2015. Retrieved six Apr 2015.
- ^ a b c Hamilos DL (October 2011). "Chronic rhinosinusitis: epidemiology and medical direction". The Journal of Allergy and Clinical Immunology. 128 (4): 693–707, quiz 708–ix. doi:ten.1016/j.jaci.2011.08.004. PMID 21890184.
- ^ a b c "Sinusitus Complications". Patient Education. University of Maryland. Archived from the original on 2010-02-22.
- ^ "Sinusitis". herb2000.com. Archived from the original on 2011-05-25.
Incidence of acute sinusitis almost ever fix in following the appearance of a cold for several days at a stretch in the person to the signal that all the profuse nasal discharge turns a distinct yellow or a dark greenish color, or perchance very thick, and foul-smelling in some cases.
[ unreliable medical source? ] - ^ a b c Ferguson M (September 2014). "Rhinosinusitis in oral medicine and dentistry". Australian Dental Journal. 59 (3): 289–95. doi:x.1111/adj.12193. PMID 24861778.
- ^ a b c DeBoer DL, Kwon E (2020). "Acute Sinusitis". Statpearls. PMID 31613481.
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License. - ^ Mehle ME, Schreiber CP (October 2005). "Sinus headache, migraine, and the otolaryngologist". Otolaryngology–Head and Neck Surgery. 133 (4): 489–96. doi:ten.1016/j.otohns.2005.05.659. PMID 16213917. S2CID 40427174.
- ^ Headache Classification Subcommittee of the International Headache Order (2004). "The International Classification of Headache Disorders: 2d edition". Cephalalgia. 24 Suppl 1 (Suppl i): 9–160. doi:10.1111/j.1468-2982.2004.00653.x. PMID 14979299.
- ^ a b c Radojicic C. "Sinusitis". Disease Direction Project. Cleveland Clinic. Archived from the original on November xiv, 2012. Retrieved November 26, 2012.
- ^ a b Terézhalmy GT, Huber MA, Jones Air conditioning, Noujeim G, Sankar V (2009). Physical evaluation in dental do . Ames, Iowa: Wiley-Blackwell. p. 27. ISBN978-0-8138-2131-3.
- ^ a b c d e f thousand h Leung RS, Katial R (March 2008). "The diagnosis and management of astute and chronic sinusitis". Primary Care. 35 (1): 11–24, v–vi. doi:10.1016/j.pop.2007.09.002. PMID 18206715.
- ^ Chandler JR, Langenbrunner DJ, Stevens ER (September 1970). "The pathogenesis of orbital complications in astute sinusitis". The Laryngoscope. eighty (9): 1414–28. doi:ten.1288/00005537-197009000-00007. PMID 5470225. S2CID 32773653.
- ^ Bakery AS (September 1991). "Role of anaerobic leaner in sinusitis and its complications". The Annals of Otology, Rhinology, and Laryngology. Supplement. 154 (9_suppl): 17–22. doi:10.1177/00034894911000s907. PMID 1952679. S2CID 13223135.
- ^ Clayman GL, Adams GL, Paugh DR, Koopmann CF (March 1991). "Intracranial complications of paranasal sinusitis: a combined institutional review". The Laryngoscope. 101 (3): 234–239. doi:10.1288/00005537-199103000-00003. PMID 2000009. S2CID 42926700.
- ^ Arjmand EM, Lusk RP, Muntz Hr (November 1993). "Pediatric sinusitis and subperiosteal orbital abscess formation: diagnosis and handling". Otolaryngology–Head and Neck Surgery. 109 (5): 886–894. doi:ten.1177/019459989310900518. PMID 8247570. S2CID 33112170.
- ^ Harris GJ (March 1994). "Subperiosteal abscess of the orbit. Age equally a factor in the bacteriology and response to treatment". Ophthalmology. 101 (3): 585–95. doi:10.1016/S0161-6420(94)31297-viii. PMID 8127580.
- ^ Dill SR, Cobbs CG, McDonald CK (Feb 1995). "Subdural empyema: analysis of 32 cases and review". Clinical Infectious Diseases. 20 (2): 372–386. doi:x.1093/clinids/twenty.2.372. PMID 7742444.
- ^ Stankiewicz JA, Newell DJ, Park AH (August 1993). "Complications of inflammatory diseases of the sinuses". Otolaryngologic Clinics of North America. 26 (4): 639–655. doi:x.1016/S0030-6665(20)30796-ix. PMID 7692375.
- ^ a b Burket'south oral medicine. Glick, Michael (12th ed.). Shelton, Connecticut. p. 341. ISBN978-one-60795-280-0. OCLC 903962852.
{{cite book}}: CS1 maint: others (link) - ^ Craig, John R.; Poetker, David M.; Aksoy, Umut; Allevi, Fabiana; Biglioli, Federico; Cha, Bruce Y.; Chiapasco, Matteo; Lechien, Jerome R.; Safadi, Ahmad; Simuntis, Regimantas; Tataryn, Roderick (2021-02-14). "Diagnosing odontogenic sinusitis: An international multidisciplinary consensus argument". International Forum of Allergy & Rhinology. eleven (8): 1235–1248. doi:10.1002/alr.22777. ISSN 2042-6976. PMID 33583151.
- ^ Saibene, Alberto Maria; Pipolo, Giorgia Carlotta; Lozza, Paolo; Maccari, Alberto; Portaleone, Sara Maria; Scotti, Alberto; Borloni, Roberto; Messina, Francesco; Di Pasquale, Daniele; Felisati, Giovanni (December 2014). "Redefining boundaries in odontogenic sinusitis: a retrospective evaluation of extramaxillary involvement in 315 patients: Odontogenic sinusitis extramaxillary interest". International Forum of Allergy & Rhinology. 4 (12): 1020–1023. doi:x.1002/alr.21400. PMID 25196643. S2CID 28835025.
- ^ Hupp JR, Ellis E, Tucker MR (2008). Gimmicky oral and maxillofacial surgery (5th ed.). St. Louis, Mo.: Mosby Elsevier. pp. 317–333. ISBN978-0-323-04903-0.
- ^ a b c d east f "Maxillary Sinusitis of Endodontic Origin" (PDF). American Association of Endodontists. 2018. Retrieved 26 March 2019.
- ^ a b Basharat U, Aiche MM, Kim MM, Sohal Yard, Chang EH (October 2019). "Are rhinoviruses implicated in the pathogenesis of sinusitis and chronic rhinosinusitis exacerbations? A comprehensive review". Int Forum Allergy Rhinol. 9 (x): 1159–1188. doi:ten.1002/alr.22403. PMID 31430424. S2CID 201117207.
- ^ Mucormycosis at eMedicine
- ^ Oral radiology : principles and interpretation. White, Stuart C.,, Pharoah, M. J. (Edition 7 ed.). St. Louis, Missouri: Elsevier. 2013-12-12. p. 475. ISBN978-0-323-09633-1. OCLC 862758150.
{{cite book}}: CS1 maint: others (link) - ^ a b c d Ahmed J, Pal S, Hopkins C, Jayaraj S (July 2011). "Functional endoscopic balloon dilation of sinus ostia for chronic rhinosinusitis". The Cochrane Database of Systematic Reviews (vii): CD008515. doi:10.1002/14651858.CD008515.pub2. PMID 21735433.
- ^ Chakrabarti A, Denning DW, Ferguson BJ, Ponikau J, Buzina Due west, Kita H, Marple B, Panda Northward, Vlaminck S, Kauffmann-Lacroix C, Das A, Singh P, Taj-Aldeen SJ, Kantarcioglu AS, Handa KK, Gupta A, Thungabathra Grand, Shivaprakash MR, Bal A, Fothergill A, Radotra BD (September 2009). "Fungal rhinosinusitis: a categorization and definitional schema addressing current controversies". The Laryngoscope. 119 (9): 1809–18. doi:10.1002/lary.20520. PMC2741302. PMID 19544383.
- ^ Boodman SG (1999-11-23). "Mayo Study on Sinusitis Draws Skeptics". The Washington Post . Retrieved 2018-06-01 .
- ^ Rank MA, Adolphson CR, Kita H (February 2009). "Antifungal therapy for chronic rhinosinusitis: the controversy persists". Current Opinion in Allergy and Clinical Immunology. 9 (1): 67–72. doi:10.1097/ACI.0b013e328320d279. PMC3914414. PMID 19532095.
- ^ Grossman J (February 1997). "One airway, one disease". Chest. 111 (2 Suppl): 11S–16S. doi:10.1378/chest.111.2_Supplement.11S. PMID 9042022.
- ^ Cruz AA (July 2005). "The 'united airways' crave an holistic approach to management". Allergy. 60 (vii): 871–four. doi:x.1111/j.1398-9995.2005.00858.x. PMID 15932375. S2CID 7490538.
- ^ Marks SC, Kissner DG (1997). "Management of sinusitis in developed cystic fibrosis". American Journal of Rhinology. eleven (ane): 11–4. doi:10.2500/105065897781446810. PMID 9065342. S2CID 5606258.
- ^ Palmer JN (December 2005). "Bacterial biofilms: do they play a role in chronic sinusitis?". Otolaryngologic Clinics of Northward America. 38 (half dozen): 1193–201, viii. doi:x.1016/j.otc.2005.07.004. PMID 16326178.
- ^ Ramadan HH, Sanclement JA, Thomas JG (March 2005). "Chronic rhinosinusitis and biofilms". Otolaryngology–Head and Neck Surgery. 132 (iii): 414–vii. doi:10.1016/j.otohns.2004.xi.011. PMID 15746854. S2CID 46197466.
- ^ Bendouah Z, Barbeau J, Hamad WA, Desrosiers M (June 2006). "Biofilm formation by Staphylococcus aureus and Pseudomonas aeruginosa is associated with an unfavorable evolution after surgery for chronic sinusitis and nasal polyposis". Otolaryngology–Head and Neck Surgery. 134 (6): 991–6. doi:10.1016/j.otohns.2006.03.001. PMID 16730544. S2CID 7259509.
- ^ Lewis K, Salyers AA, Taber HW, Wax RG, eds. (2002). Bacterial Resistance to Antimicrobials. New York: Marcel Decker. ISBN978-0-8247-0635-vii. Archived from the original on 2014-01-07.
- ^ Sanclement JA, Webster P, Thomas J, Ramadan HH (April 2005). "Bacterial biofilms in surgical specimens of patients with chronic rhinosinusitis". The Laryngoscope. 115 (4): 578–82. doi:10.1097/01.mlg.0000161346.30752.18. PMID 15805862. S2CID 25830188.
- ^ Pearlman AN, Conley DB (June 2008). "Review of electric current guidelines related to the diagnosis and treatment of rhinosinusitis". Current Stance in Otolaryngology & Caput and Cervix Surgery. xvi (three): 226–thirty. doi:x.1097/MOO.0b013e3282fdcc9a. PMID 18475076. S2CID 23638755.
- ^ a b c Rosenfeld RM, Andes D, Bhattacharyya Due north, Cheung D, Eisenberg S, Ganiats TG, Gelzer A, Hamilos D, Haydon RC, Hudgins PA, Jones S, Krouse HJ, Lee LH, Mahoney MC, Marple BF, Mitchell CJ, Nathan R, Shiffman RN, Smith TL, Witsell DL (September 2007). "Clinical practice guideline: adult sinusitis". Otolaryngology–Head and Cervix Surgery. 137 (3 Suppl): S1-31. doi:10.1016/j.otohns.2007.06.726. PMID 17761281. S2CID 16593182.
- ^ Ebell MH, McKay B, Dale A, Guilbault R, Ermias Y (March 2019). "Accurateness of Signs and Symptoms for the Diagnosis of Acute Rhinosinusitis and Acute Bacterial Rhinosinusitis". Annals of Family Medicine. 17 (two): 164–172. doi:10.1370/afm.2354. PMC6411403. PMID 30858261.
- ^ Folio 674 Archived 2017-02-16 at the Wayback Motorcar in: Flint Prisoner of war, Haughey BH, Niparko JK, Richardson MA, Lund VJ, Robbins KT, Lesperance MM, Thomas JR (2010). Cummings Otolaryngology – Head and Cervix Surgery, 3-Volume Set. Elsevier Health Sciences. ISBN9780323080873.
- ^ Harrison's Manual of Medicine xvi/e
- ^ a b c d e f g Consumer Reports; American Academy of Family unit Physicians (April 2012). "Treating sinusitis: Don't rush to antibiotics" (PDF). Choosing wisely: an initiative of the ABIM Foundation. Consumer Reports. Archived (PDF) from the original on June 11, 2012. Retrieved August 17, 2012.
- ^ American University of Allergy, Asthma, and Immunology. "5 things physicians and patients should question" (PDF). Choosing Wisely: an initiative of the ABIM Foundation. American Academy of Allergy, Asthma, and Immunology. Archived (PDF) from the original on November 3, 2012. Retrieved August fourteen, 2012.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ a b c Consumer Reports; American Academy of Allergy, Asthma, and Immunology (July 2012), "Treating sinusitis: Don't rush to antibiotics" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, Consumer Reports, archived (PDF) from the original on January 24, 2013, retrieved August 14, 2012
{{citation}}: CS1 maint: multiple names: authors list (link) - ^ Lemiengre MB, van Driel ML, Merenstein D, Liira H, Mäkelä M, De Sutter AI (September 2018). "Antibiotics for astute rhinosinusitis in adults". The Cochrane Database of Systematic Reviews. 2018 (ix): CD006089. doi:10.1002/14651858.CD006089.pub5. PMC6513448. PMID 30198548.
- ^ Harvey R, Hannan SA, Badia Fifty, Scadding G (July 2007). Harvey R (ed.). "Nasal saline irrigations for the symptoms of chronic rhinosinusitis". The Cochrane Database of Systematic Reviews (3): CD006394. doi:x.1002/14651858.CD006394.pub2. PMID 17636843.
- ^ Rhinitis medicamentosa at eMedicine
- ^ Shaikh N, Wald ER (October 2014). "Decongestants, antihistamines and nasal irrigation for acute sinusitis in children". The Cochrane Database of Systematic Reviews. 10 (ten): CD007909. doi:10.1002/14651858.CD007909.pub4. PMC7182143. PMID 25347280.
- ^ Zalmanovici Trestioreanu A, Barua A, Pertzov B (May 2018). "Cyclamen europaeum extract for acute sinusitis". The Cochrane Database of Systematic Reviews. five (8): CD011341. doi:ten.1002/14651858.CD011341.pub2. PMC6494494. PMID 29750825.
- ^ Head K, Precipitous S, Chong LY, Hopkins C, Philpott C (September 2018). "Topical and systemic antifungal therapy for chronic rhinosinusitis". The Cochrane Database of Systematic Reviews. 2018 (nine): CD012453. doi:10.1002/14651858.cd012453.pub2. PMC6513454. PMID 30199594.
- ^ a b Lemiengre MB, van Driel ML, Merenstein D, Liira H, Mäkelä M, De Sutter AI (September 2018). "Antibiotics for acute rhinosinusitis in adults". Cochrane Database Syst Rev. 2018 (ix): CD006089. doi:10.1002/14651858.CD006089.pub5. PMC6513448. PMID 30198548.
- ^ Smith SR, Montgomery LG, Williams JW (March 2012). "Treatment of mild to moderate sinusitis". Archives of Internal Medicine. 172 (six): 510–3. doi:10.1001/archinternmed.2012.253. PMID 22450938.
- ^ Karageorgopoulos DE, Giannopoulou KP, Grammatikos AP, Dimopoulos Thousand, Falagas ME (March 2008). "Fluoroquinolones compared with beta-lactam antibiotics for the treatment of acute bacterial sinusitis: a meta-assay of randomized controlled trials". CMAJ. 178 (7): 845–54. doi:ten.1503/cmaj.071157. PMC2267830. PMID 18362380.
- ^ a b Grub AW, Benninger MS, Beck I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick G, Volturo G, Wald ER, File TM (April 2012). "IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults". Clinical Infectious Diseases. 54 (eight): e72–e112. doi:10.1093/cid/cir1043. PMID 22438350.
- ^ "Fluoroquinolone Antibacterial Drugs: Drug Safety Advice – FDA Advises Restricting Use for Certain Elementary Infections". FDA. 12 May 2016. Archived from the original on 16 May 2016. Retrieved 16 May 2016.
- ^ Falagas ME, Karageorgopoulos DE, Grammatikos AP, Matthaiou DK (February 2009). "Effectiveness and safety of short vs. long duration of antibiotic therapy for acute bacterial sinusitis: a meta-analysis of randomized trials". British Journal of Clinical Pharmacology. 67 (2): 161–71. doi:10.1111/j.1365-2125.2008.03306.x. PMC2670373. PMID 19154447.
- ^ Williamson IG, Rumsby Chiliad, Benge S, Moore Chiliad, Smith Prisoner of war, Cross M, Little P (December 2007). "Antibiotics and topical nasal steroid for handling of astute maxillary sinusitis: a randomized controlled trial". JAMA. 298 (21): 2487–96. doi:x.1001/jama.298.21.2487. PMID 18056902.
- ^ Zalmanovici Trestioreanu A, Yaphe J (December 2013). "Intranasal steroids for acute sinusitis". The Cochrane Database of Systematic Reviews. 12 (12): CD005149. doi:x.1002/14651858.CD005149.pub4. PMC6698484. PMID 24293353.
- ^ Hayward G, Heneghan C, Perera R, Thompson M (2012). "Intranasal corticosteroids in direction of acute sinusitis: a systematic review and meta-assay". Annals of Family unit Medicine. 10 (iii): 241–9. doi:10.1370/afm.1338. PMC3354974. PMID 22585889.
- ^ Chong LY, Caput Chiliad, Hopkins C, Philpott C, Schilder AG, Burton MJ (Apr 2016). "Intranasal steroids versus placebo or no intervention for chronic rhinosinusitis". The Cochrane Database of Systematic Reviews. 4: CD011996. doi:ten.1002/14651858.cd011996.pub2. PMID 27115217.
- ^ Chong LY, Head K, Hopkins C, Philpott C, Burton MJ, Schilder AG (April 2016). "Different types of intranasal steroids for chronic rhinosinusitis". The Cochrane Database of Systematic Reviews. 4: CD011993. doi:10.1002/14651858.cd011993.pub2. PMID 27115215.
- ^ Head Grand, Chong LY, Hopkins C, Philpott C, Burton MJ, Schilder AG (Apr 2016). "Short-class oral steroids solitary for chronic rhinosinusitis". The Cochrane Database of Systematic Reviews. 2016 (4): CD011991. doi:x.1002/14651858.cd011991.pub2. PMC8504433. PMID 27113367.
- ^ a b Fokkens W, Lund V, Mullol J (2007). "European position newspaper on rhinosinusitis and nasal polyps 2007". Rhinology. Supplement. 20 (one): 1–136. doi:10.1017/S0959774306000060. PMID 17844873. S2CID 35987497.
- ^ Thomas M, Yawn BP, Cost D, Lund 5, Mullol J, Fokkens W (June 2008). "EPOS Primary Intendance Guidelines: European Position Paper on the Primary Care Diagnosis and Direction of Rhinosinusitis and Nasal Polyps 2007 - a summary". Master Care Respiratory Journal. 17 (two): 79–89. doi:10.3132/pcrj.2008.00029. PMC6619880. PMID 18438594.
- ^ Venekamp RP, Thompson MJ, Hayward G, Heneghan CJ, Del Mar CB, Perera R, et al. (March 2014). "Systemic corticosteroids for acute sinusitis" (PDF). The Cochrane Database of Systematic Reviews (3): CD008115. doi:ten.1002/14651858.CD008115.pub3. PMID 24664368.
- ^ Head K, Chong LY, Hopkins C, Philpott C, Schilder AG, Burton MJ (April 2016). "Short-course oral steroids every bit an adjunct therapy for chronic rhinosinusitis". The Cochrane Database of Systematic Reviews. 4: CD011992. doi:10.1002/14651858.cd011992.pub2. PMID 27115214.
- ^ Tichenor WS (2007-04-22). "FAQ — Sinusitis". Archived from the original on 2007-eleven-01. Retrieved 2007-10-28 .
- ^ Rimmer J, Fokkens W, Chong LY, Hopkins C (1 Dec 2014). "Surgical versus medical interventions for chronic rhinosinusitis with nasal polyps". The Cochrane Database of Systematic Reviews. 12 (12): CD006991. doi:10.1002/14651858.CD006991.pub2. PMID 25437000.
- ^ Sharma R, Lakhani R, Rimmer J, Hopkins C (November 2014). "Surgical interventions for chronic rhinosinusitis with nasal polyps". The Cochrane Database of Systematic Reviews (11): CD006990. doi:10.1002/14651858.cd006990.pub2. PMID 25410644.
- ^ Stammberger H (February 1986). "Endoscopic endonasal surgery--concepts in treatment of recurring rhinosinusitis. Part I. Anatomic and pathophysiologic considerations". Otolaryngology–Head and Cervix Surgery. 94 (two): 143–7. doi:10.1177/019459988609400202. PMID 3083326. S2CID 34575985.
- ^ Liang J, Lane AP (March 2013). "Topical Drug Delivery for Chronic Rhinosinusitis". Current Otorhinolaryngology Reports. 1 (1): 51–sixty. doi:10.1007/s40136-012-0003-4. PMC3603706. PMID 23525506.
- ^ Anon JB (April 2010). "Upper respiratory infections". The American Periodical of Medicine. 123 (4 Suppl): S16-25. doi:10.1016/j.amjmed.2010.02.003. PMID 20350632.
- ^ Dykewicz MS, Hamilos DL (Feb 2010). "Rhinitis and sinusitis". The Journal of Allergy and Clinical Immunology. 125 (2 Suppl 2): S103-15. doi:x.1016/j.jaci.2009.12.989. PMID 20176255.
External links [edit]
- Sinusitis at Curlie
- "Sinusitis". MedlinePlus. U.Southward. National Library of Medicine.
Source: https://en.wikipedia.org/wiki/Sinusitis
0 Response to "Can You Have a Sinus Infection Without Mucus"
ارسال یک نظر